Resources
2022 Physician Compensation Report
Regardless of your specialty or what city you work in, most physicians are curious about how their salary stacks up against the competition.
Whether you’re thinking about practicing in a new state or wondering if your signing bonus is on par with what it should be, know the facts to protect yourself and your annual earnings.
Let’s answer some questions about:
- Which physicians make the most money?
- Moving a few states away to increase your salary?
- How your specialty compares against the salaries of physicians in other areas of medicine?
- How much physicians are really making
- Which specialties are in the greatest demand
- Which regions of the country are hiring the most
- Where physicians are being offered the biggest bonuses
Spending hours pouring through hundreds of pages in pricey compensation reports is usually the only way to find this information — but we did the legwork for you.
We have created our annual physician compensation report to save you both time and money looking for the data and statistics you want to know.
In this report, we detail:
- How physicians in different medical specialties and regions of the United States are being compensated for their work
- The gender wage gap
- How much physicians are earning in bonuses and incentives
- Which specialties are in the greatest demand
We’ve compiled data from nearly a dozen different sources from data made available as of 2021 to offer you:
The Free Physicians Thrive 2022 Physician Compensation Report
Physicians’ salaries vary by region, specialty, gender, and a variety of other factors. From year to year, we see increases in certain regions, increases in salary for certain specialties, and increasing bonuses in areas where the demand for physicians is the highest.
We’ve broken down the compensation trends for physicians by specialty, region, gender, and by bonus incentives to provide insight into where salaries are increasing and where they’re decreasing.
Compensation by Region
Large and mid-sized metro areas, where there are more medical institutions and more medical professionals, continue to pay some of the lowest salaries.
Rural areas, which tend to have a more difficult time recruiting top-tier talent, continue to pay some of the highest salaries in the country.
There are, however, some mid-sized metro areas that saw a salary increase. Five of the ten are located in the Southeast region of the U.S.
Metro areas with the biggest salary increases:
- Providence +8.9%
- Portland, OR +8.6%
- Richmond, VA +7.5%
- Las Vegas +7.2%
- New Orleans +7.2%
- Birmingham +6.9%
- Atlanta +6.8%
- Denver +6.7%
- Salt Lake City +6.5%
- Jacksonville +6.3%
Metro areas that pay the highest salaries:
- Milwaukee: $430,274
- Atlanta: $428,244
- Jacksonville: $427,090
- Buffalo: $407,070
- Orlando: $406,587
- Raleigh: $406,365
- Charlotte: $404,285
- Minneapolis: $401,978
- Riverside, CA: $397,005
- Dallas: $396,184
Metro areas that pay the lowest salaries:
- San Antonio: $329,475
- Virginia Beach: $331,952
- Boston: $347,894
- Baltimore: $348,389
- Washington D.C: $351,272
- Denver: $352,073
- Philadelphia: $354,788
- Memphis: $356,875
- Louisville: $360,609
- Providence: $365,807
In addition to having more medical professionals overall, the metro areas paying the smallest salaries have a few other things in common.
Many of them have older healthcare infrastructures as well as plateauing populations. This is especially the case with cities on the eastern seaboard, such as D.C., Baltimore, Philadelphia, and Boston, as large groups of people are moving out of these more expensive cities in favor of more affordable cities in the South and Midwest.
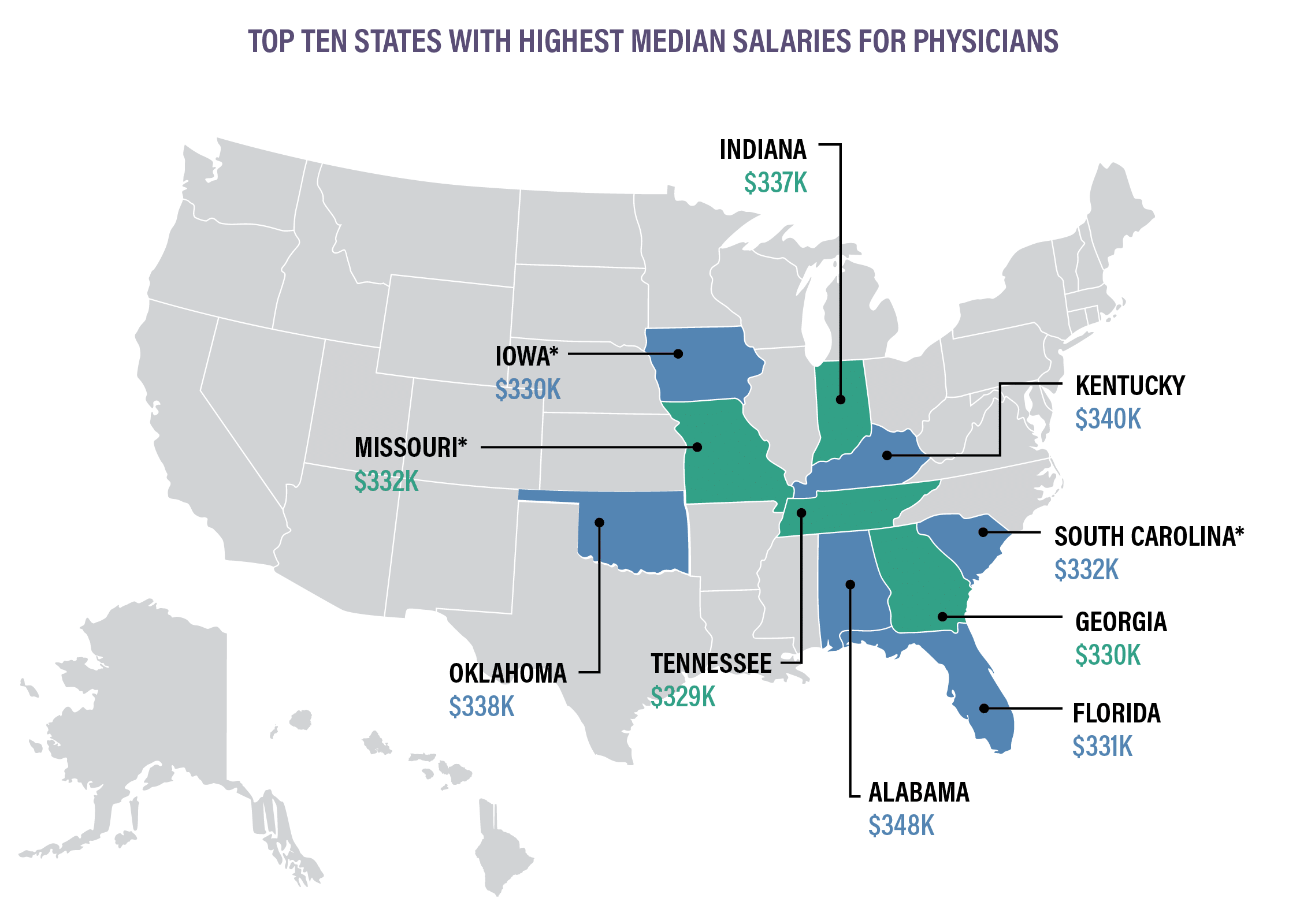
*Indicates states that are new to the top ten for 2020. These states replaced Utah, Ohio, and North Carolina.
Physicians in rural areas are earning higher salaries than those in metropolitan areas. Data shows that physicians across the highest-paying specialties are earning more in rural regions:
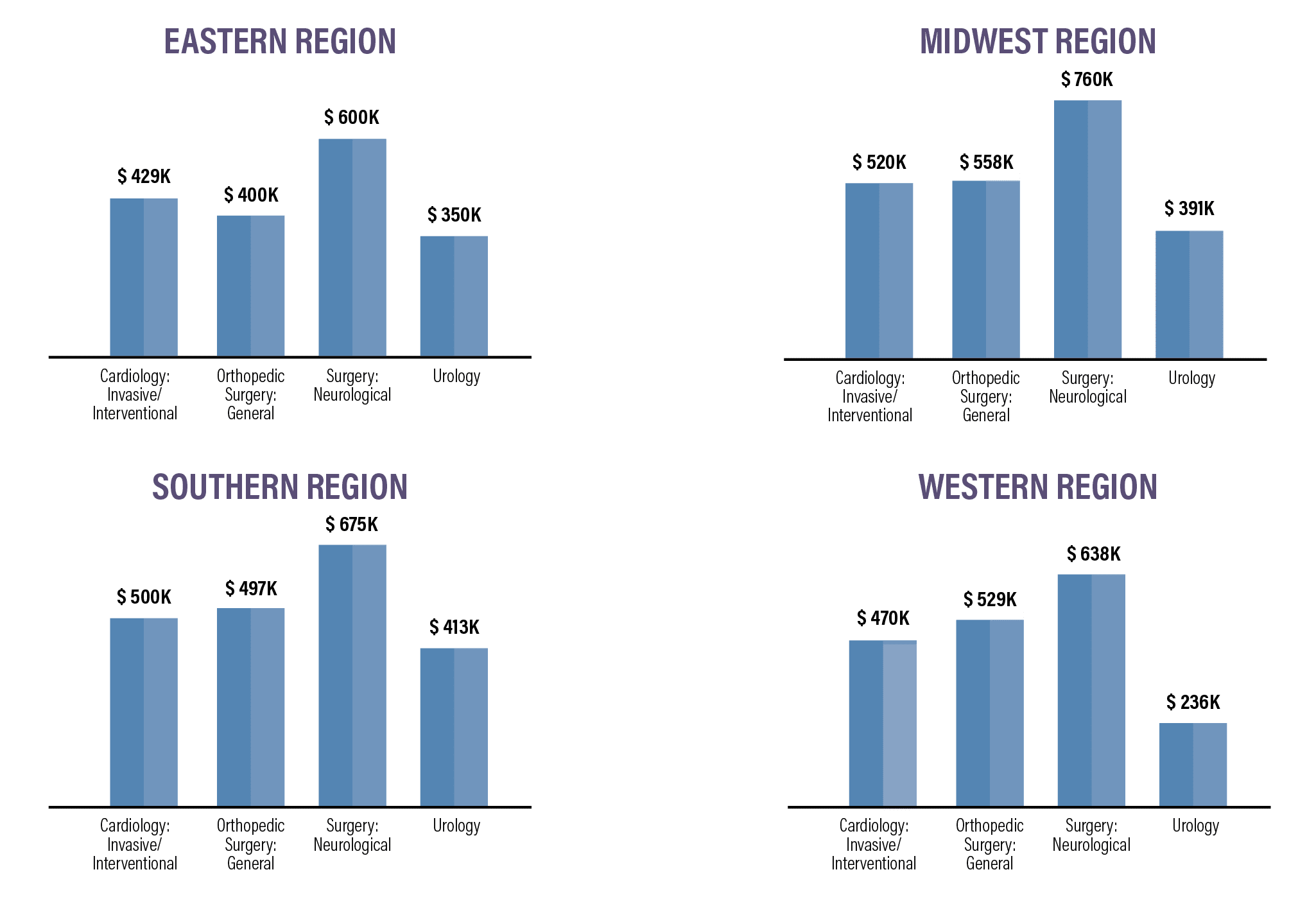
Overall, the Midwest and the South make the most, while physicians on the East and West coasts earn the least. There are a variety of reasons for this variation in pay, with the higher concentration of qualified physicians in the Northeast region continuing to be one of the most significant.
PCPs earned an average of $242k in 2021, down slightly from $243k in 2020. Specialists earned an average of $344k in 2021, down from $346k in 2020.Surgical specialists continue to be among some of the highest-paid professionals in medicine. Pediatricians and those who practice family medicine continue to be among the lowest-paid physicians.
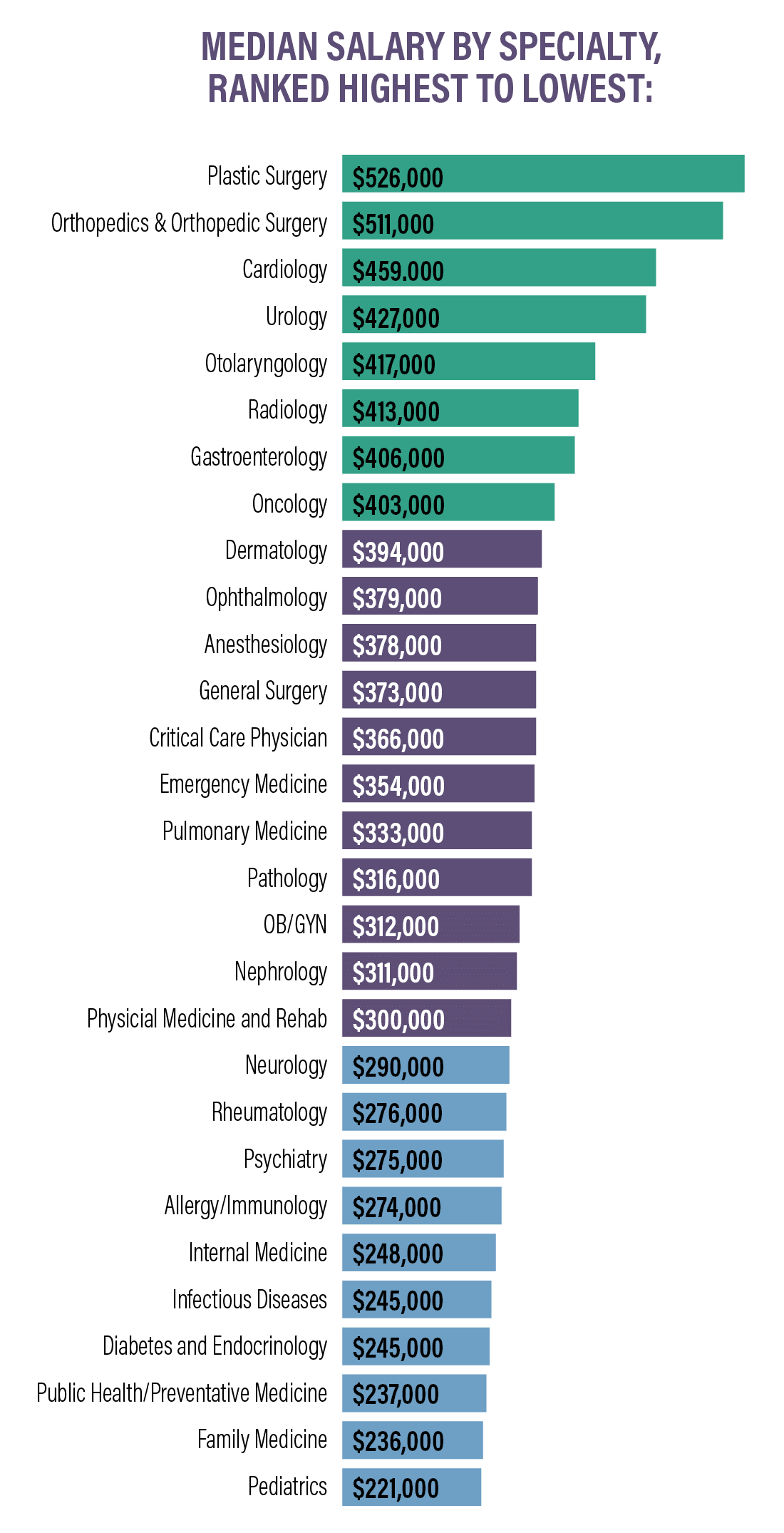
Specialties with the biggest salary increases:
- Plastic Surgery +10%
- Oncology +7%
- Rheumatology +5%
- Cardiology +5%
- Diabetes and Endocrinology +4%
Specialties with the biggest salary decreases:
- Allergy/Immunology -9%
- Otolaryngology -9%
- Anesthesiology -5%
- Pediatrics -5%
- Dermatology -4%
Plastic surgeons and orthopedic surgeons are the highest earners and are the only specialties with an average compensation of over $500,000.
Compensation by Gender
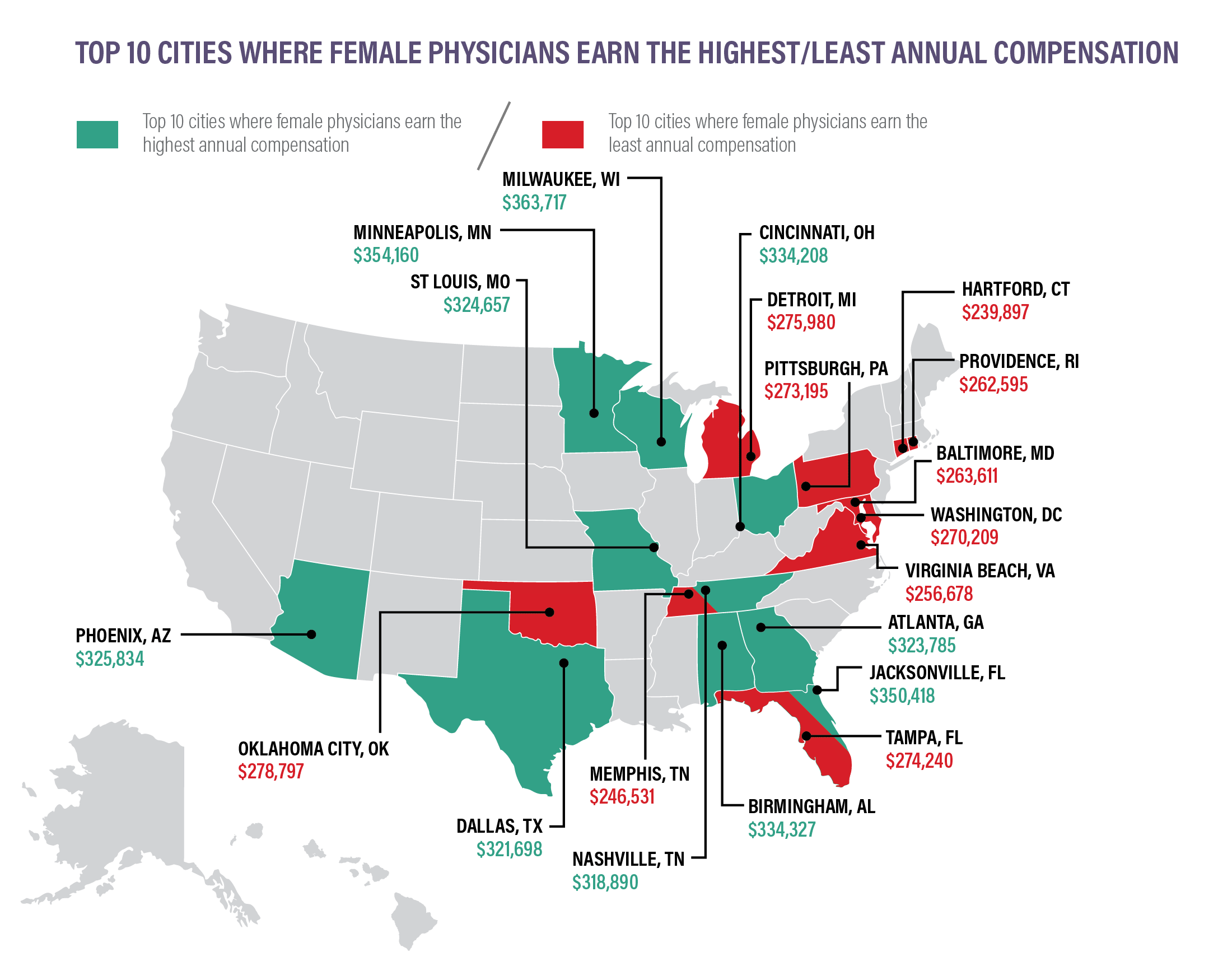
As in most professions, there continues to be a pay gap based solely on gender in the U.S.
Data shows that in primary care, men earn $269k per year, while women earn just $211k, approximately 22% less than their male counterparts. The gap is slightly larger in specialty medicine, with male specialists earning $376k per year and women specialists earning $283k (a difference of approximately 25%).
So, where do women earn the most and earn the least? Where is the gender wage gap most prevalent?
Our findings show that the gender pay gap varies considerably based on region and specialty.
Specialties with the largest gender wage gaps:
- Otolaryngology: women earn 22% less
- Geriatrics: women earn 21.4% less
- Orthopedic surgery: women earn 20% less
- Research: women earn 19.8% less
- OBGYN: women earn 19.6% less
Specialties with the smallest gender wage gaps:
- Nuclear medicine: women earn 2.5% less
- Hematology: women earn 11.4% less
- Urology: women earn 12% less
- Colon/Rectal surgery: women earn 12.2% less
- Emergency medicine: women earn 12.6% less
Related: How Female Physicians can Counteract the Gender Pay Gap
Compensation Bonuses
Physicians in both primary care and specialties continue to earn bonuses, but there has been a shift away from RVU-based production bonuses in favor of net collections bonuses.
There was also a large decrease in the quality-based bonus system.
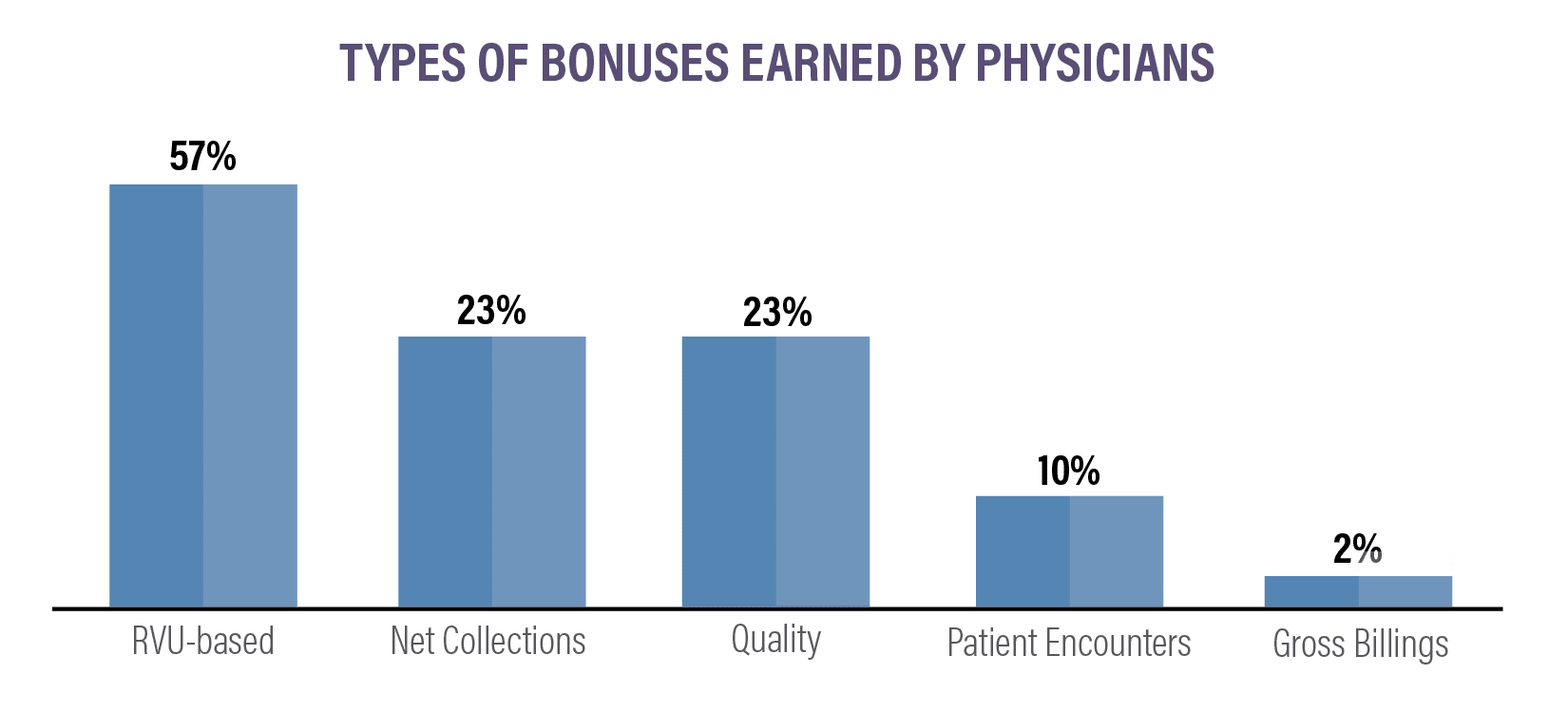
In 2021, here’s how bonuses compared to the previous year:
- RVU-based: 57% (down from 73% last year)
- Net collections: 23% (up from 13% last year)
- Gross billings: 2% (same as last year)
- Patient encounters: 10% (down from 12% last year)
- Quality: 23% (down from 64% last year)
Average incentive bonus by specialty:
- Orthopedics/Orthopedic surgery: $116k
- Ophthalmology: $87k
- Otolaryngology: $72k
- Urology: $72k
- Cardiology: $71k
- Radiology: $69k
- Gastroenterology: $60k
- Anesthesiology: $55k
- OBGYN: $48k
- General surgery: $47k
- Emergency medicine: $44k
- Pathology: $42k
- Critical care unit physician: $41k
- Neurology: $39k
- Physical medicine/rehab: $37k
- Family medicine: $27k
- Internal medicine: $26k
- Pediatrics: $26k
- Psychiatry: $24k
Amongst specialists, 55% reported earning an incentive bonus in 2021. Amongst PCPs, 59% received an average incentive bonus of $27k.
Since the beginning of the COVID-19 pandemic, certain types of practices and employment settings have seen more growth than others, with multi-specialty group practices experiencing the most growth, and government settings seeing the least:
- Multi-specialty group: 4.1%
- Health maintenance organization: 3.9%
- Industry/pharmaceutical: 3.8%
- Health system/IDN/ACO: 2.7%
- Single specialty group: 2.3%
- Urgent care center/chain: 2.1%
- Solo practice: 1.6%
- Academic: 1.2%
- Hospital: 1.1%
- Government: 0.6%
Related: When Physicians Should Walk Away From a Job Offer
Compensation Trends Summary
Here are the key takeaways:
- Primary care physicians earned an average of $242k in 2021, down from $243k in 2020.
- Specialists earned an average of $344k in 2021, down from $346k in 2020.
- Physicians in the Midwest earn the highest salaries; physicians in the East earn the least.
- Plastic surgery, orthopedics, and orthopedic surgery, and cardiology are the three highest-earning specialties.
- The biggest salary increases are in plastic surgery and oncology.
- The biggest salary decreases are in allergy/immunology and otolaryngology.
- On average, female physicians earn 25% less than male physicians in the same specialty.
- 55% of specialists earned an incentive bonus.
- 59% of PCPs earned an incentive bonus.
- Multi-specialty group practices saw the biggest growth of any practice setting, at 4.1%.
Hiring Trends
Certain types of physicians are in much greater demand than others. In addition, certain regions are in much greater need of top-quality physicians.
We’ve compiled data from medical recruiting firms and other sources to create a breakdown of hiring trends based on specialty, region, and medical setting.
Hiring Trends by Specialty
For the past 13 years, family physicians have been the most heavily recruited physicians around the country. But with COVID-19 causing a decrease in office visits, 2021 created an increase in specialist recruiting for the first time in over a decade.
Top 10 Most Recruited Physicians:
- Hematologists/Oncologists
- Radiologists
- Neurologists
- Gastroenterologists
- Psychiatrists
- Dermatologists
- Endocrinologists
- Cardiologists
- Family Medicine Specialists
- Obstetricians/Gynecologists
Many of these specialties top the recruitment list because they generated some of the highest amounts of revenue for hospitals and practices.
With a focus on mental health and the stress caused to so many by the pandemic, psychiatry saw the fourth-highest engagement of any medical specialty this year.
There is still a continuing shortage of physicians across the board and a projected shortage throughout the next decade.
Projected deficit of physicians through 2025:
- Cardiology: 7,080
- Ophthalmology: 6,180
- Orthopedic surgery: 5,050
- Urology: 3,630
- General surgery: 2,970
- Cardiothoracic surgery: 1,800
- Gastroenterology: 1,630
- Hematology/oncology: 1,400
- Pulmonology: 1,400
- Neurological surgery: 1,200
There is also a growing shortage of physicians, nurse practitioners (NPs), and physician assistants (PAs) across the country.
By 2030, the overall shortage of physicians in the United States is expected to reach 121,300. Of that 121,300, approximately 55,200 are primary care physicians and 67,000 are specialists, spread out among a wide variety of specialties.
Hiring Trends by Region
The Eastern part of the country and most major metropolitan areas have the greatest number of trained physicians. Midwestern and Southern states, which have the largest aging populations, continue to face the most significant shortages. This directly corresponds to why physicians in these states often receive higher salaries and larger bonuses.
The pandemic continues to affect the growth of medical practices. Here’s how recruitment trends have shifted, based on employment setting, in the past year:
- Hospital recruitment: 33% in 2021 (up from 26% in 2020)
- Medical group recruitment: 29% in 2021 (up from 28% in 2020)
- Academic medical center recruitment: 20% in 2021 (up from 18% in 2020)
- Federally qualified health center recruitment: 8% in 2021 (up from 6% in 2020)
- Physician recruitment for solo, partnership, and concierge practices remained unchanged at 3% in 2021 and 2020.
Some employment settings also prove riskier in terms of average salary. Here’s how the average salary varies by employment setting for some of the top-earning specialists:
Orthopedic Surgery (General)
- Single specialty: $535k
- Multi-specialty: $480k
- Rural Health Clinic: $600k
- Federally Qualified Health Center: $521k
- Academic Department: $364k
Cardiology (Invasive-Interventional)
Urology
- Single specialty: $550k
- Multi-specialty: $435k
- Hospital Department Practice: $450k
- Rural Health Clinic:$520k
- Academic Department: $236k
- Single specialty: $305k
- Multi-specialty: $419k
- Hospital Department Practice: $400k
- Federally Qualified Health Center: $406k
- Academic Department: $281k
The biggest factors causing physician shortages:
- Aging population (population over age 65 expected to grow 48% by 2032)
- Overall population growth (expected to grow 10% by 2032)
- A large amount of older physicians nearing retirement age
- Rural and low-income urban areas are expected to see the greatest shortage
- States with aging populations, such as the Midwest and South, are also expected to see the greatest shortages
It’s important to note that new recruits are being denied some benefits that were standard before the pandemic.
In 2019/2020, 97% of all recruitment offers included relocation expenses. For 2020/2021, only 74% of new offers included relocation expenses.
CME offers remained relatively stable, with 94% of new offers receiving CME payments this year, down from 96% last year.
While relocation expenses have been scaled back, the following benefits are up across the board for new hires:
- Health insurance: 78% (up from 67% last year)
- Malpractice: 76% (up from 67% last year)
- Retirement/401k: 68% (up from 63% last year)
- Disability: 70% (up from 58% last year)
Hiring Trends Summary
Here are the key takeaways:
- There is a shortage of physicians, particularly in the Midwest and Southern regions.
- The demand for physicians is expected to increase.
- Rural and underserved areas pay the highest salaries and the biggest bonuses.
- For the first time in over a decade, family physicians are no longer the most recruited physicians.
The Impact of COVID-19 on Physicians Salaries and Satisfaction
COVID-19 has had significant impacts on the healthcare industry. While hospitals are crowded with patients, physicians outside of hospital settings have experienced major decreases in appointments.
Forty-four percent of physicians believe that the reduction in patient visits will continue even after COVID, and that they could continue to have up to 25% less visits than they did prior to the pandemic. Ten percent of physicians expect COVID to have an even greater impact, and believe they will see visits drop by 26% or more as compared to pre-COVID visits.
Forty-six percent of physicians are more optimistic and expect that patient volume will return to normal after the pandemic.
Physicians report having experienced the following situations in their workplace setting since the beginning of COVID-19:
- 72% have experienced a reduction in income
- 43% have had to work with reduced staff
- 8% have had to close their practice
The pandemic has taken a serious toll on physicians’ lives outside of work as well. Physicians report experiencing the following:
- Burnout: 58%
- Feelings of anger and/or anxiety: 50%
- Withdrawing from family and friends: 43%
- Sought medical attention for a mental health issue: 13%
More than 33% of physicians surveyed have also expressed a desire to retire in the next year.
Would Physicians Choose the Same Specialty Again?
If given the chance to change careers, 78% of physicians said they would choose to work in medicine again. Of those, some specialists are more satisfied with their choice of specialty than others.
Physicians most likely to choose the same specialty again:
- Dermatology: 96%
- Orthopedics/Orthopedic Surgery: 96%
- Oncology: 96%
- Ophthalmology: 94%
- Otolaryngology: 93%
- Radiology: 93%
- Gastroenterology: 93%
- Urology: 92%
- Plastic Surgery: 92%
- Cardiology: 92%
Physicians Least Likely to Choose the Same Specialty Again
- Public Health/Preventative Medicine: 67%
- Internal Medicine: 68%
- Family Medicine: 71%
- OBGYN: 74%
- Nephrology: 77%
- Critical Care Unit Physician: 78%
- Emergency Medicine: 79%
- Diabetes/Endocrinology: 81%
- Pediatrics: 82%
- Pulmonary Medicine: 83%
How Many Hours Are Physicians Working?
Physicians are working almost the same amount of hours now as they were prior to COVID-19. Many physicians were furloughed, and there was a reduction in patient volume, but most physicians report that they are working an average of 51 hours per week, up from 50 hours per week prior to COVID-19.
The breakdown of how many hours physicians spend on patient care versus paperwork varies significantly depending on specialty. Physicians in the infectious diseases field spend 24.2 hours per week on paperwork alone, and those in public health/preventative medicine spend 20.7 hours per week.
Ophthalmologists and anesthesiologists spend the least amount of time on paperwork, averaging just over 10 hours per week.
Are Physicians Happy?
For many physicians, the work is rewarding and their salary is fair. But are physicians actually happy with their job? Data shows that many physicians don’t feel as though they are being fairly compensated and that they are dissatisfied with many aspects of the job.
Aspects of the job that physicians find the most rewarding:
- Helping others: 26%
- Relationships with patients: 26%
- Finding answers, diagnoses: 24%
- Earning the salary: 12%
- Being proud to be a physician: 5%
- Teaching: 4%
- Other: 2%
- Nothing: 2%
Aspects of the job that physicians like the least:
- Having so many rules and regulations: 23%
- Working long hours: 14%
- Difficult patients: 14%
- Difficulty getting reimbursement: 12%
- Working on an EHR system: 11%
- Worrying about being sued: 7%
- Danger/risk of treating COVID-19 patients: 7%
- Other: 9%
- Nothing: 3%
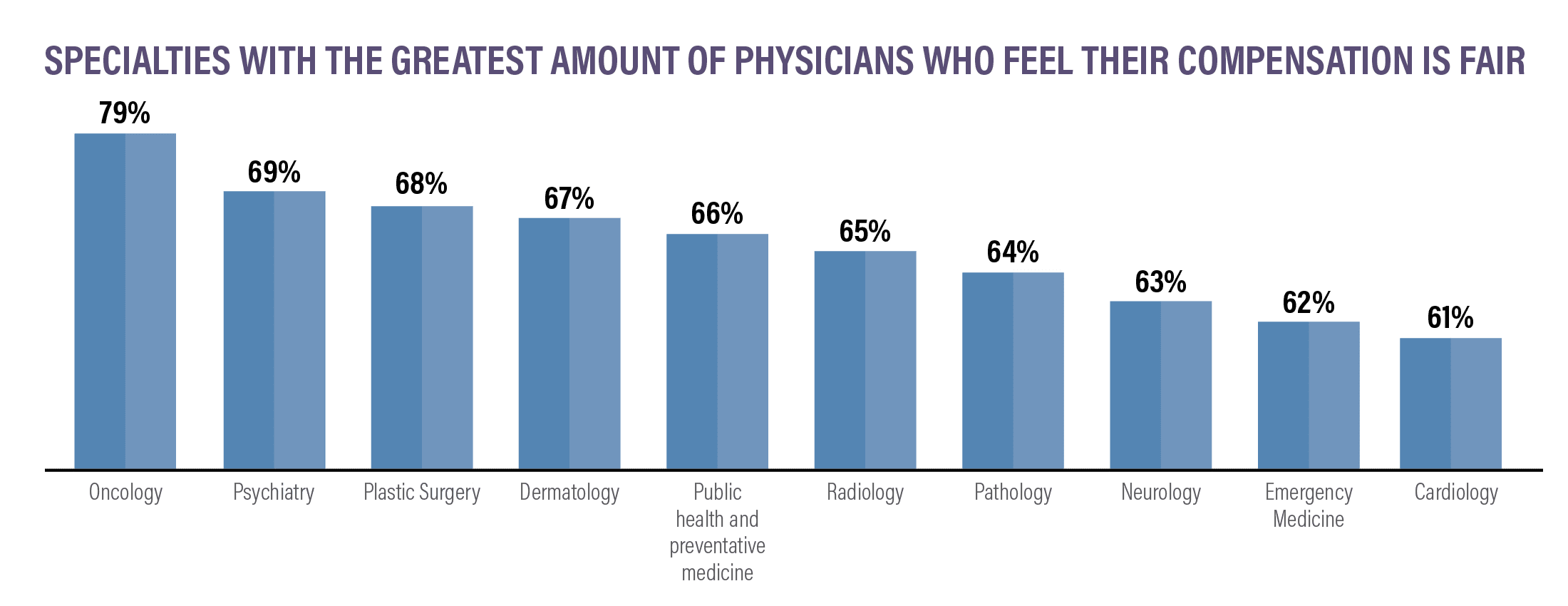
While many physicians are satisfied with their professions and their salaries, burnout is still common in the medical profession.
In addition to the stress that COVID-19 has put on the healthcare system, long hours, dealing with the bureaucracy of hospital administrations, and working on primitive electronic health records (EHR) systems remain some of the main contributors to their dissatisfaction.
About to sign a physician contract for the first time?
Conducting a job search in a new state?
Wondering how your incentives and bonuses stack up against those in other specialties?
This report shows a broad picture of compensation and hiring trends to help physicians gather industry data and analyze the current healthcare landscape, no matter where they are in their careers.
Note that these are averages and are not set in stone. To understand your market value for your specialty and region, talk with one of our expert contract review specialists. We can help you negotiate the salary and incentives you deserve.
To hire a contract review specialist, discuss financial planning for retirement, find creative tax-saving solutions, or protect your finances with disability insurance or life insurance, contact Physicians Thrive now.