Key Takeaways
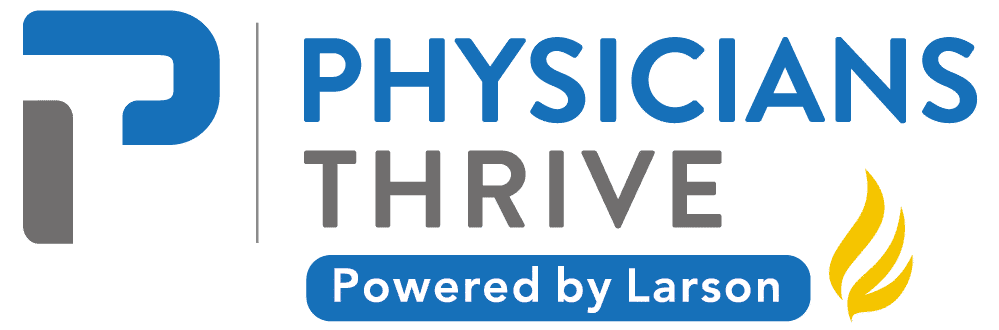
- Medical practice management involves financial planning, patient coordination, HR, billing, and compliance.
- Effective management streamlines workflows, improves patient care, and boosts practice revenue.
- Physicians often lack business training, requiring skilled management or specialized consultant support.
- Achieving practice success demands practical experience, ongoing education, and targeted professional development.
Being a successful medical practice manager is wholly different from being a good physician.
Countless physicians believed that their medical skills were enough to open their own practice in the healthcare industry.
While this is often true, they miss the “business” aspect of things, potentially dooming their practice before it even begins.
You can choose to learn medical practice management or have someone qualified to do it for you.
Either way, you’ll need this guide to fully understand what’s going on.
Table of Contents
What Is Medical Practice Management?
While there’s no official definition, medical practice management is the art of running a healthcare business, including scheduling appointments, managing patient records, and billings.
It also includes a variety of operational tasks, like budgeting, staffing, organizing, etc.
Here is the complete list of duties performed by a medical practice manager:
Financial Management
Managing finances is easily the cornerstone of any successful medical practice.
It involves budget planning, expense monitoring, and revenue cycle management to ensure financial viability.
Financial management can start with a simple Excel sheet, which requires a lot of manual data entry but can be useful to help small practices save some money.
However, as patient numbers increase, there will be no way around automating the financial management aspect using dedicated tools.
Managing Patient Records
Another vital component is managing accurate and secure patient records.
This includes ensuring compliance with state and federal regulations regarding data privacy, such as HIPAA.
Plus, proper management of patient records enhances the quality of care by providing professionals with quick and easy access to patient information whenever needed.
Human Resources
Human resources are a little tricky in the healthcare system since they require specialized approaches to talent acquisition, development, and retention within the constantly changing variables of the medical field.
Because of the small margin of error in the field, you can’t just hire anyone whose resume says that they’re capable, you’ll need to have the following:
- Healthcare-specific recruitment strategies.
- Compliance-focused onboarding and training.
- Compensation structure development.
- Performance management systems.
- Professional development and continuing education.
Medical Billing
Once again, working in medicine takes the simple process of pricing a service to a different level.
It’s a complicated process that requires precise coding, thorough documentation, and meticulous follow-up to ensure appropriate compensation for provided services.
A good medical billing strategy should have these elements:
- ICD-10 and CPT coding accuracy.
- Patient billing and collection with compliance monitoring.
- Billing staff training and development.
- Claims submission and tracking.
Patient Care Coordination
Coordinating patients is in no way an easy feat. On paper, everyone gets assigned an appointment that they should stick to.
In reality, people can be late or even forget the appointment entirely.
Decent care coordination must allow for some leniency between appointments to prevent long waiting times or overlapping of appointments.
Even then, some patients may wait considerably longer if the doctor spends a long time with a patient with a complicated condition.
The coordinator should anticipate such cases by checking the patient history.
There are also follow-ups, referrals, chronic diseases, etc.
Multiply it by the number of doctors within the practice, and things can get overwhelming quickly.
Accordingly, a successful care coordination plan encompasses:
- Treatment plan coordination.
- Chronic disease management programs.
- Referral management systems.
- Care gap identification and resolution.
- Patient education delivery.
Modern medical practices rely heavily on technology to support these functions through:
- Electronic health record (EHR) systems.
- Telehealth platforms.
- Data security protocols.
- Practice management software.
- Mobile health applications.
- Analytics and reporting tools.
Patient Experience Management
Great marketing brings patients, but it’s the patient’s experience that will retain or repulse them from coming back.
Accordingly, satisfaction has become a critical metric for healthcare organizations, influencing everything from reimbursement rates to online reputation.
To achieve such satisfaction, medical practices should focus on:
- Comfort amenities.
- Communication protocols.
- Feedback collection mechanisms.
- Waiting time management.
- Service recovery procedures.
- Brand experience consistency.
Related: Practice Management Services
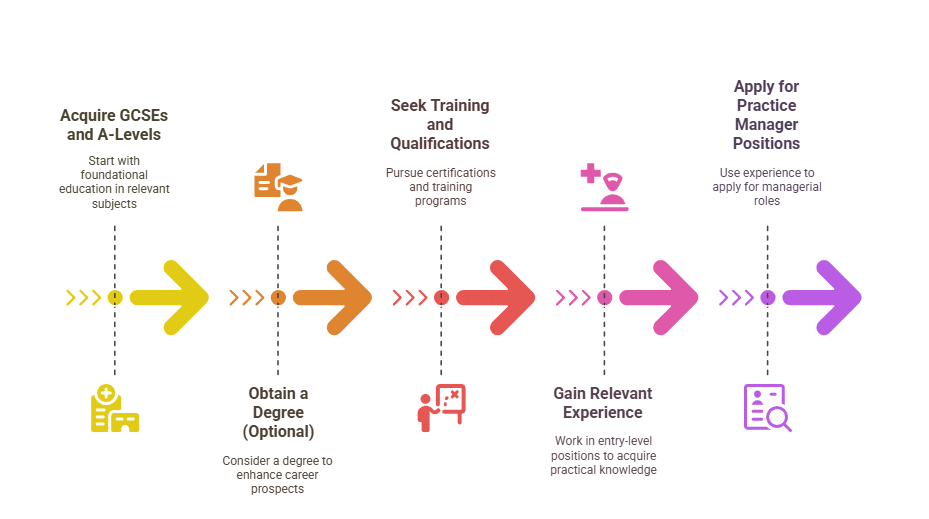
How to Become a Medical Practice Manager
Here’s the whole process of becoming a medical practice manager:
Step 1: Acquire GCSEs and A-Levels
You need to start by getting the proper educational foundation, typically by acquiring GCSEs and A-levels related to business or healthcare.
Step 2 (Optional): Get a Degree
Although not strictly required, obtaining a degree can significantly boost your prospects.
Consider a degree in fields like business management, healthcare administration, human resources, or finance.
Step 3: Seek Training and Qualifications
Step 3 can be an alternative or a supplemental step to step 2. Various training programs and certifications can help you gain the necessary skills.
Look for courses offered by organizations like the Association of Medical Secretaries, Practice Managers, Administrators, and Receptionists ( AMSPAR) or the Institute of Health and Social Care Management ( IHSCM).
Step 4: Gain Relevant Experience
Like any other field, you’ll need to gain experience, which means working in entry-level positions within a medical practice.
Don’t be discouraged by the initial low payment; everyone starts there.
Plus, this hands-on experience will help you understand the day-to-day operations of a medical office that you simply can’t acquire unless you experience it outside theoretical books.
Step 5: Apply for Practice Manager Positions
Once you gain enough experience, you may begin applying for practice manager roles.
At this point, it becomes a process of smartly filling your CV with all your experience using the currently accepted ATS approach.
Manage Your Practice With Physicians Thrive
It’s hard to find an online guide that includes everything you need to know about medical practice management. Such a guide simply doesn’t and won’t exist.
You may not be aware of your next step.
- Should you learn how to manage your own practice or hire medical office managers to do so?
- Do you even have the budget for that?
- What about your student loans and other expenses?
You may have countless other questions in mind, but trust that Physicians Thrive will have all the answers you’ll need, plus some more.
All you have to do is decide to work with us. We offer a series of focused services for anything medical.
In short words, if you’re a physician, we can help.