Whether you work as an employee of a large hospital group or own a private practice, CPT codes play an essential role in all physicians’ lives. Regardless of your specialty and the type of patient care you deliver, it’s crucial you understand all about those five-digit codes.
As a physician, CPT codes may not be your primary focus or something that you’ve given much thought. However, they are an unavoidable part of the job.
From knowing which codes to use and how they affect your bottom line, here’s what physicians need to know about CPT codes.
Table of Contents
Why Are CPT Codes So Important?
CPT codes are Current Procedural Terminology codes used in every area of medicine.
CPT coding streamlines medical billing practices across the country and ensures that inpatient and outpatient procedures get billed consistently across all hospitals and practices.
Whether you practice radiology, cardiology, or any other subspecialty, physicians use CPT codes in every sector of the healthcare industry.
CPT codes identify every medical service you provide and every patient procedure you conduct. A CPT code is required in order to indicate the service provided and receive reimbursement from payers. This is true whether your patients have Medicare, private health insurance, or employer-provided insurance.
There are three categories of CPT codes:
- Category I codes describe services and procedures
- Category II codes track follow up care and outcomes
- Category III codes note when a physician uses an emerging technology
The American Medical Association annually updates the complete list of CPT codes. They add new codes every year, and old codes get dropped or changed. Physicians and medical practices must always stay up to date with the current years’ codes.
Fail to use the proper CPT codes, and insurance companies can reject claims and deny reimbursement. Ultimately, the CPT codes you bill will determine how much you earn.
See also: How Much Disability Insurance do Physicians Need?
CPT Codes and RVUs
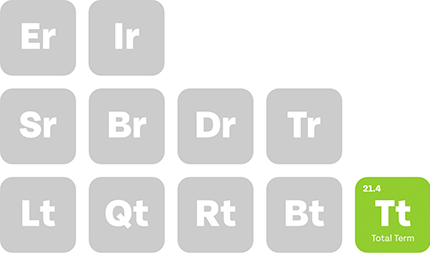
How exactly do CPT codes affect your earnings? Every CPT code becomes tied to a relative value unit (RVU).
Medicare assigns and determines the RVU, and it is that RVU that determines the reimbursement amount that physicians receive. To understand why the CPT code is important, it’s crucial to understand the factors that go into determining the RVU.
The first component of the RVU is the wRVU. This is the work relative value unit, which accounts for the amount of time, skill, and effort it takes to perform a specific procedure or provide a particular service.
The second component is the practice expense RVU. This considers the cost of overhead, including office space, medical equipment, and office supplies.
The third component is the professional liability RVU. This component factors in the cost that the physician pays for malpractice insurance premiums.
The fourth component is the Geographic Practice Cost Index, or GPCI. This figure modifies the other components’ values based on the cost of living in each particular geographic area. For example, the GCPI for physicians in New York City is higher than that of physicians throughout New York state, as the cost of living in NYC is much greater than in other parts of the state.
The final determining factor is called the conversion factor. Because Medicare is a federal program, the United States Congress determines a conversion factor based on the Medical Economic Index. The conversion factor changes from year to year.
Total RVU
For physicians in private practice, knowing how to calculate RVUs is crucial to your bottom line. Ensure that every physician and everyone responsible for patient billing in your practice knows why CPT codes are essential.
They must take the required steps to check that CPT codes do not get misused, overlooked, or eliminated in the billing process.
Related: Physician Practice Disability: BOE Reimbursement
CPT Codes and wRVUs
For physicians in private practice, the RVU of a service directly affects how much revenue the practice earns. For physicians who work as employees, the most crucial component of the CPT code is the wRVU.
As described above, the wRVU reflects the amount of time, skill, and effort a physician puts into providing patient care. And for many physicians who work as employees of large hospital groups, the wRVU primarily determines your salary.
If you don’t use the right code, you could log less wRVUs than you’re actually doing. This will result in earning less money for the services you provided and deserve pay.
Examples
Here are some examples of similar codes and how their wRVUs vary.
Codes 99214 and 99215 refer to an established patient office visit. The 99214 code is a level 4 code used for a standard 20-25 minute office visit, while the 99215 code is a level 5 code used for a routine 30-45 minute office visit.
And while the length of the visit only varies slightly, the wRVUs assigned to these codes are quite different. The 2020 Medicare Physician Fee Schedule gives the 99214 code a wRVU of 1.5. The 99215 code has a wRVU of 2.11.
Another example of similar CPTs with varying wRVUs is codes 99495 and 99496, both of which refer to transitional care management. Code 99495 has a wRVU of 2.36, while code 99496 has a wRVU of 3.1.
Codes G0438 and G0439, which denote initial annual wellness visits and subsequent annual wellness visits, are similar yet have very different wRVUs. Code G0438 has a wRVU of 2.43, whereas code G0439 has a wRVU of 1.5.
These are but a few examples of how using the wrong code, even when similar, can significantly affect your total earnings and revenue.
See also: The Definitive Guide to wRVU Physician Compensation
Always Use the Right CPT Code
Using the wrong CPT code doesn’t just affect your earnings; it can cause other adverse outcomes as well.
Coding errors can harm a patient’s care. If you bill a patient under the wrong code and their insurance only pays a part of the reimbursement, insurance could leave them with a larger portion of the bill to pay. This may cause patients not to seek subsequent or follow-up treatment, for fear of incurring another hefty bill.
Using the wrong codes can also delay or prevent reimbursement from Medicare, Medicaid, and private health insurers.
Consistent usage of the wrong CPT codes may even result in a fraud investigation. If there is evidence of fraud in medical billing, you may incur a fine or, worse yet, lose your license to practice medicine. Federal law requires all healthcare providers to follow the current medical code set at all times.
To ensure that you’re using the proper CPT codes on every bill, retain access to the current AMA code set. From 2019 to 2020, the AMA’s CPT Editorial Panel added 248 codes, deleted 71 existing codes, and amended 75 others.
Telehealth and online services are recent additions to the code set, as are codes explicitly related to the testing of COVID-19.
Protect your patients, your revenue, and your practice by ensuring that all of your medical coders have access to the current code list.
Be Wary of CPT Codes With Modifiers
As if CPT codes weren’t confusing enough, some services require that you add a modifier. These modifiers are additional descriptors that help provide extra details and information about specific procedures.
Many physicians have a negative view of specific modifiers — and with just cause. Some commonly used modifiers can negatively impact the wRVU of a procedure.
Here are a few of the most common modifiers used in CPT billing that can reduce your wRVU:
- Modifier 51: indicates you performed an addition procedure to the originally-coded one
- Modifier 62: indicates that two surgeons were present during a surgical procedure
- Modifier 76: indicates that it’s a repeat procedure
- Modifier 80: indicates that there was an assistant surgeon present during a surgical procedure
By law, you must indicate all relevant modifiers whenever and wherever they apply.
For more on modifiers, read our post on The Basics of CPT Conversions with Modifiers.
Physicians Can Increase Revenue by Evaluating Their Billing Process
Inaccurate CPT coding can have significant negative consequences on your practice and your annual earnings.
Ensure that your billing process is accurate, up to date, and monitored in a way that will bring in revenue with these four steps:
1. Evaluate Your Current System
It is best practice to evaluate and re-evaluate billing sheets annually. Also, take proactive measures to ensure that you are not missing billing opportunities.
It doesn’t matter whether you’re providing diagnostic services, practicing family medicine, or performing surgery. Every healthcare provider can benefit from analyzing their current systems and ensuring the efficient handling of their billing procedures.
2. Identify Missed Opportunities
An analysis of your current procedures may indicate that there are certain services you’re not consistently billing. Look for missed opportunities and areas where you may be accidentally missing codes that you’re entitled to use.
Transitional care management, chronic care management, and advanced care planning are three areas where many physicians are short-changing themselves by overlooking important CPT codes.
3. Know Who’s Coding
You must know who is overseeing your billing and coding procedures. Many physicians assign CPT codes themselves, but your employer may also grant a medical coder or biller the authority to change them.
Make sure that you know who is authorized to change your CPT codes. Ensure that that person or team is up to date on all aspects of the current CPT code set and ICD codes and HCPCS codes. A medical coder who doesn’t know the best practices and procedures could cause you to lose revenue with every single patient visit.
It’s also important for physicians to be active in their reviews. Keep a log of your CPT codes and wRVUS as you see patients. At the end of the week or month, compare your record to the reports from your coder or biller. This is the best way to ensure accuracy, identify inconsistencies, and receive the compensation you deserve.
Provide Coders With the Proper Resources
There are many resources that coders can use to ensure billing accuracy and proper coding.
SpeedECoder, SuperCoder, ACS Coding Today, and EncoderPro are just a few of the existing software programs that coders can use to ensure they are using the proper CPT codes for every patient and procedure.
A CPT frequency report can be helpful, as well. It will identify all of the CPT codes billed by a specific physician in a given period. A CPT frequency report is a great tool that can give you a quick snapshot of your billing practices. It can also see which codes you use most often and identify opportunities where you may be able to make use of other codes with higher wRVUs.
And, above all else, make sure your coders have access to the most up-to-date CPT codes. The AMA released the new 2021 CPT code set in September of 2020. Between 2020 and 2021, they added 206 new codes, deleted 54 others, and revised 69 additional codes.
Similar: Alternative Tax-Free Income for Physicians
Conclusion
It is the responsibility of every health care professional to ensure that they’re using the proper CPT codes at all times. Failure to use the right procedure codes can result in a claim denial, reimbursement delay, and a decrease in your overall earnings.
Whether you own your practice or work as an employee, it’s time to take CPT coding seriously. As a practicing physician, you must be aware that if you ignore CPT codes, they can negatively affect your bottom line.
Interested in discussing your physician contact review, tax planning, or other services that protect your bottom line? Contact Physicians Thrive today.
Subscribe to our email newsletter for expert tips about finances, insurance, employment contracts, and more!